Liver Disease And Clotting Factors
Liver disease and clotting factors. Primary hemostasis coagulation and. The high rate of hemorrhage has been previously recognized. 2 Assessment of true bleeding risk in.
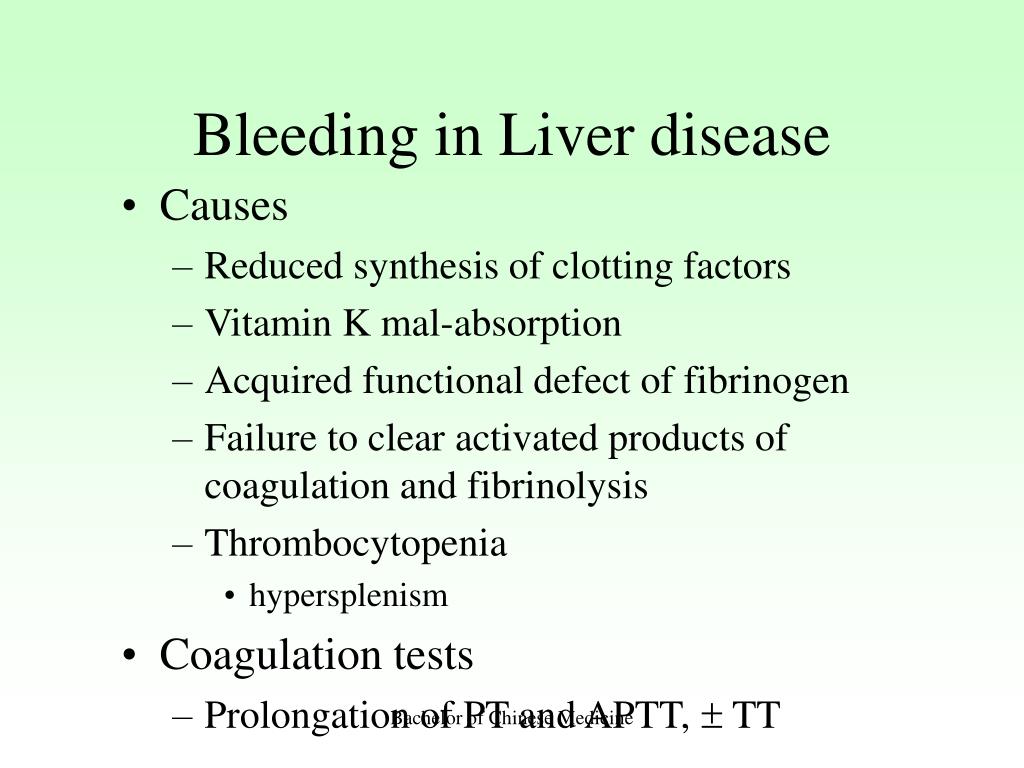
Liver disease results in complex alterations of all 3 phases of hemostasis. Liver disease is associated with impairment of the haemostatic function due to the abnormal and decreased synthesis of the clotting factors. Exposure of vWF from an endothelial breach activates platelets leading to platelet aggregation.
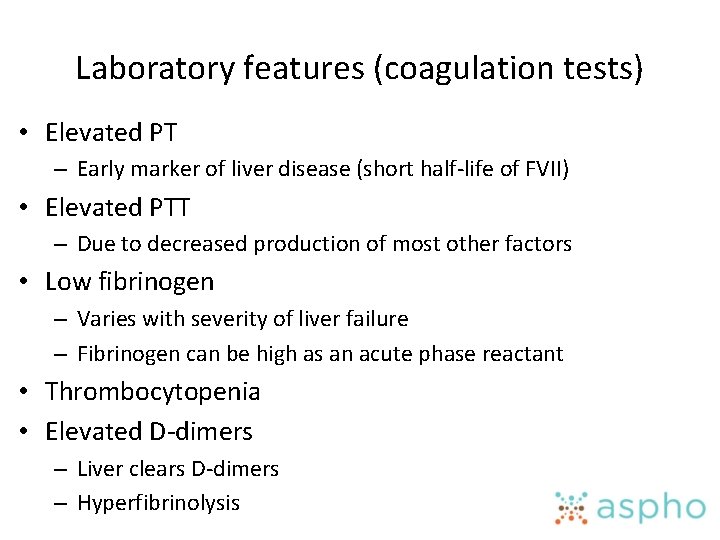
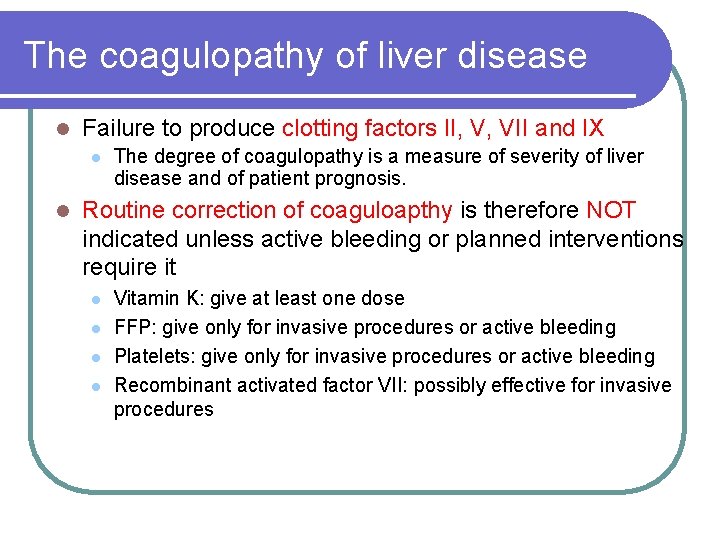
Severe liver injury leads to reduction of liver synthesis of clotting factors and consequently prolonged PT or an increased INR which is a method to homogenize PT level reporting across the world. It is thus only logical to have considered assessment of the clotting profile to include prothrombin time PT and activated partial thromboplastin time aPTT to be an integral part of the comprehensive assessment of a patient who presents with liver impairment. The liver produces multiple proteins involved in the normal clotting process including coagulation factors fibrinogen and plasminogen.
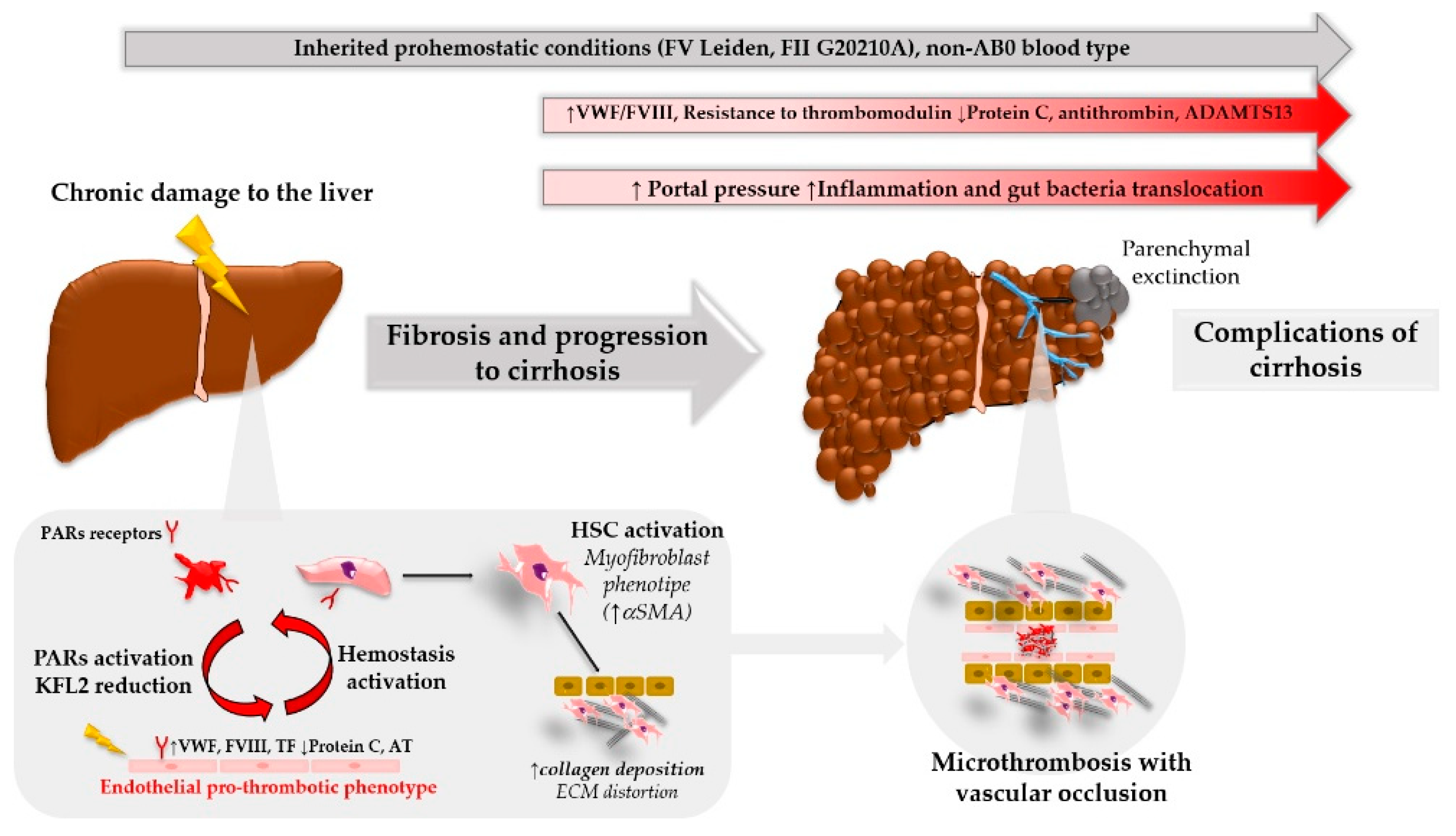
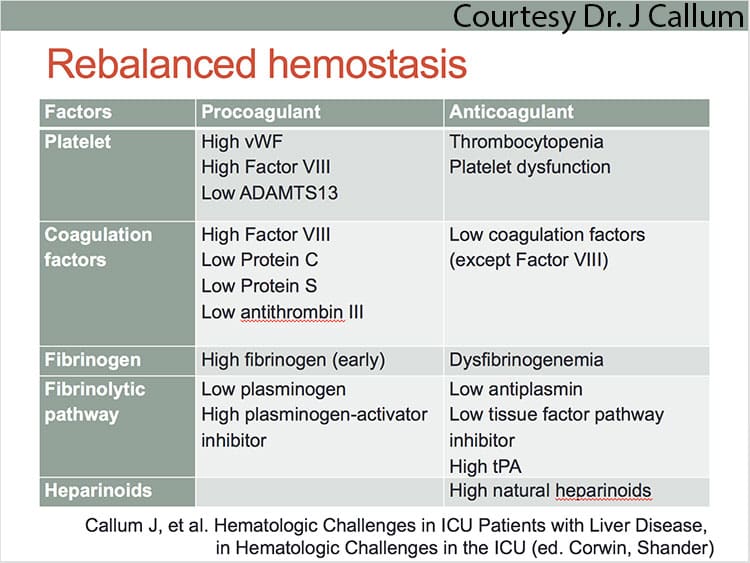
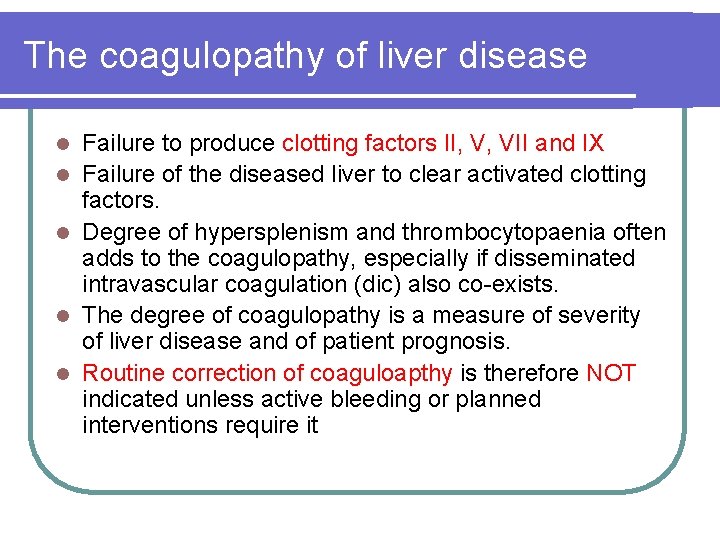
However the increased risk for thrombosis is only more recently being appreciated. The liver produces the majority of coagulation proteins needed in blood clotting cascade. Decreased synthesis of clotting and inhibitor factors decreased clearance of activated factors quantitative and qualitative platelet defects hyperfibrinolysis and accelerated intravascular coagulation.
Factor VII is created by the vascular endothelium. Vitamin K deficiency may coexist resulting in defective carboxylation of clotting factors and inhibitors. Liver disease is associated with impairment of the haemostatic function due to the abnormal and decreased synthesis of the clotting factors.
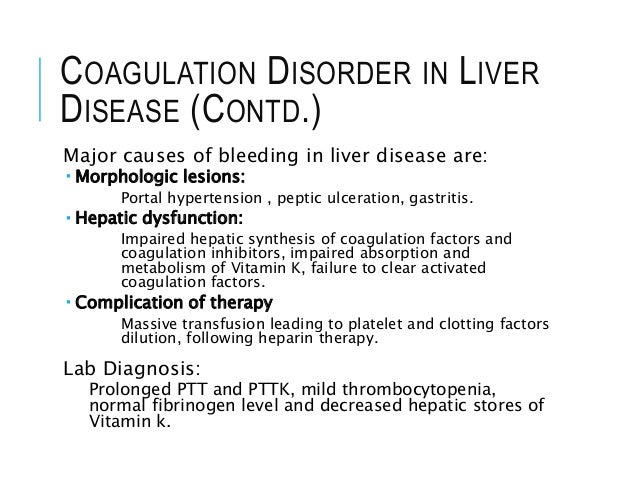
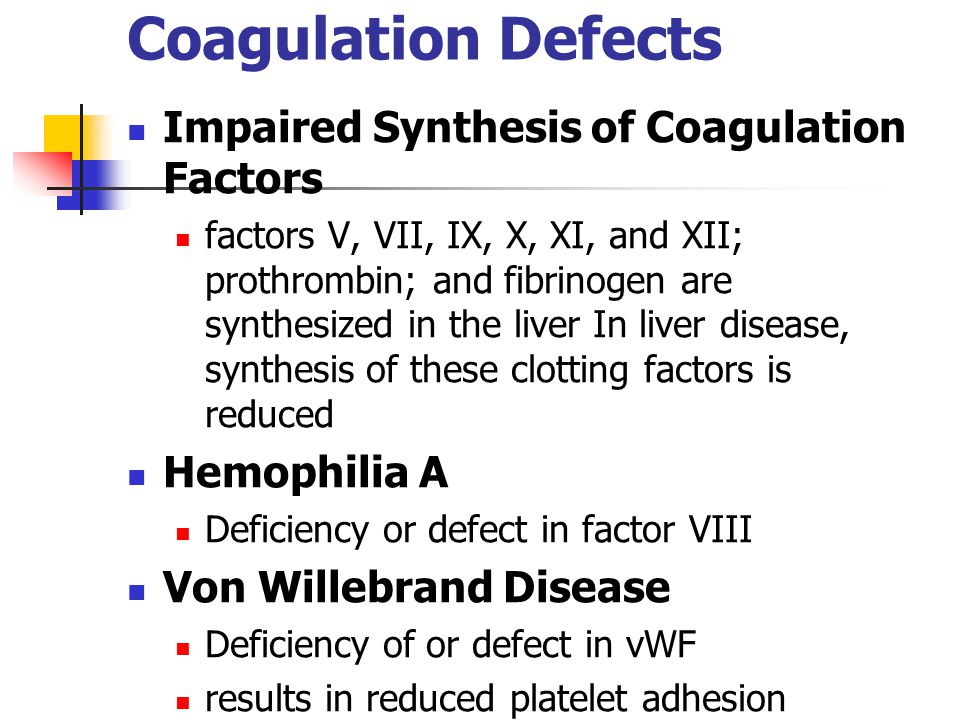
This is undertaken because of the misconception that a prolonged PT in a patient with liver disease presumably because of multiple coagulation-factor deficiencies is associated with an increased risk of bleeding and giving vitamin K will help by increasing vitamin K-dependent clotting factors. These include factors II V VII IX X XI and XII. 1 The complex interplay in liver disease can disrupt the prohemostatic and antihemostatic factors thus leading to a disruption in the balance of bleeding and clotting in patients with chronic liver disease.
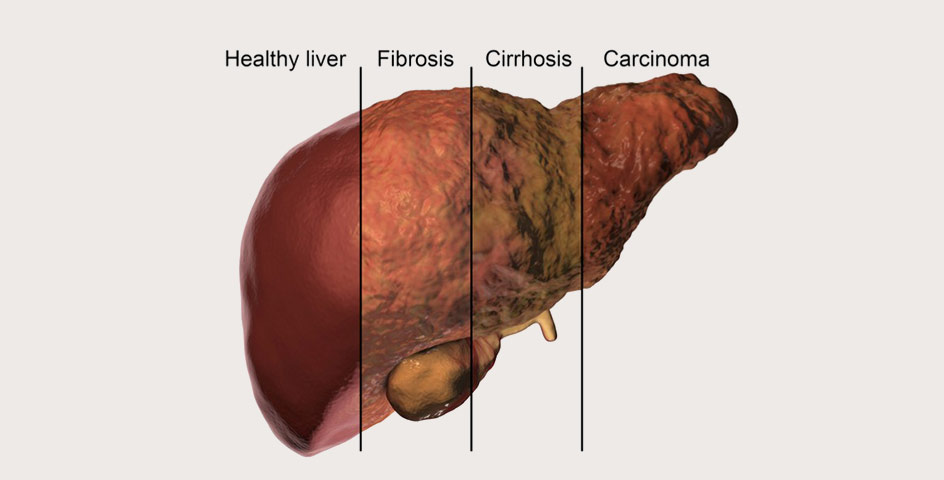
Nonetheless there are major alterations in the hemostatic pathways in most patients with liver disease including altered platelet and endothelial function altered clotting factors and conditions such as hyperfibrinolysis dysfibrinogenemia and renal failure which may be superimposed on these underlying abnormalities. The liver is the first organ exposed to all molecules from the intestines and the increased hepatic inflammation caused by increasedchanges in exposure to bacterial byproducts or metabolites due to either intestinal edema or changes in the gut microbiota and maybe especially trimethylamine N-oxide TMAO which are also produced in the liver and associated with both HF and liver disease.
The liver plays a central role in the clotting process and acute and chronic liver diseases are invariably associated with coagulation disorders due to multiple causes.
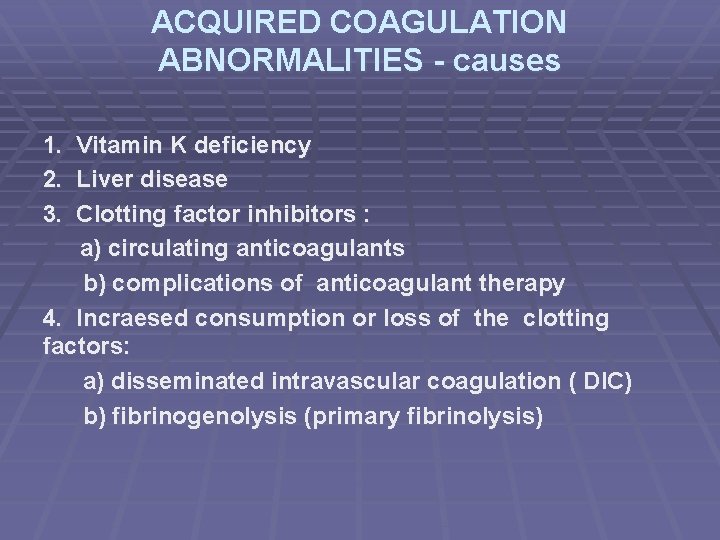
Coagulation abnormalities in liver disease. This is primarily related to abnormal clotting of blood caused by a reduced ability of the liver to synthesise clotting factors. The high rate of hemorrhage has been previously recognized. The liver plays a central role in the clotting process and acute and chronic liver diseases are invariably associated with coagulation disorders due to multiple causes. Decreased synthesis of clotting and inhibitor factors decreased clearance of activated factors quantitative and qualitative platelet defects hyperfibrinolysis and accelerated intravascular coagulation. Factor VII is created by the vascular endothelium. Liver disease is associated with impairment of the haemostatic function due to the abnormal and decreased synthesis of the clotting factors. Several other causes may also contribute to hemostatic defects in liver disease patients such as thrombocytopenia alterations in platelet and endothelial cell functions clotting factors. Severe liver injury leads to reduction of liver synthesis of clotting factors and consequently prolonged PT or an increased INR which is a method to homogenize PT level reporting across the world.
Liver disease is associated with impairment of the haemostatic function due to the abnormal and decreased synthesis of the clotting factors. The liver is the first organ exposed to all molecules from the intestines and the increased hepatic inflammation caused by increasedchanges in exposure to bacterial byproducts or metabolites due to either intestinal edema or changes in the gut microbiota and maybe especially trimethylamine N-oxide TMAO which are also produced in the liver and associated with both HF and liver disease. All coagulation factors but VIII which is mainly produced by the endothelium are markedly reduced in patients with liver disease. The liver produces the majority of coagulation proteins needed in blood clotting cascade. The extent of coagulation abnormalities depends upon the degree. The high rate of hemorrhage has been previously recognized. Primary hemostasis coagulation and.





























Post a Comment for "Liver Disease And Clotting Factors"